Tips on Managing Heat & Diabetes This Summer
 Summertime brings in warmer temperatures, lengthier days, and increased outdoor activities. Treating Type 1 or Type 2 diabetes during this time of year requires careful planning and attention for those managing diabetes. Excessive heat, sun exposure, and changes to routine present unique challenges to managing blood sugar and general well being. There are a few ways to effectively manage your diabetes this summer. Our tips will help you maintain hydration, navigate outdoor activities and safeguard your skin.
Summertime brings in warmer temperatures, lengthier days, and increased outdoor activities. Treating Type 1 or Type 2 diabetes during this time of year requires careful planning and attention for those managing diabetes. Excessive heat, sun exposure, and changes to routine present unique challenges to managing blood sugar and general well being. There are a few ways to effectively manage your diabetes this summer. Our tips will help you maintain hydration, navigate outdoor activities and safeguard your skin.
Heat Related Risks for Diabetics
Dehydration
High temperatures can lead to excessive sweating, increasing the risk of dehydration. Dehydration can cause elevated blood glucose levels and potentially lead to diabetic ketoacidosis (DKA) in individuals with Type 1 diabetes. In Type 2 diabetes, dehydration can also affect blood sugar control.
Heat Exhaustion and Heatstroke
People with diabetes are more susceptible to heat exhaustion and heatstroke due to impaired sweating mechanisms or autonomic neuropathy. Heat exhaustion can cause symptoms like fatigue, dizziness, nausea, and headaches. Heatstroke is a severe condition that can be life-threatening and requires immediate medical attention.
Hypoglycemia
Heat and sun exposure can affect insulin absorption, leading to a higher risk of hypoglycemia (low blood sugar). Heat can make insulin work more rapidly, so it's essential to monitor blood sugar levels closely and adjust insulin dosages as necessary. You may need to pack extra vials of insulin depending on your activity. Protect your insulin vials from getting damaged or broken with silicone cases. Sweating and increased physical activity during summer can also increase the risk of hypoglycemia.
Foot Care
Prolonged sun exposure and heat can increase the risk of foot complications, especially for individuals with diabetes-related nerve damage (neuropathy) or poor circulation. It is important to protect the feet from direct sunlight, wear proper footwear, and conduct regular foot inspections to identify any signs of injury or infection.
Medication Storage
Extreme heat can impact the effectiveness and stability of insulin and certain diabetes medications. It's crucial to store insulin and medications properly, away from direct sunlight and at the recommended temperature range. When traveling, use an insulated diabetes supply bag to keep medications at the appropriate temperature.
Skin Complications
Diabetes can increase the risk of skin complications, and sun exposure can exacerbate these issues. People living with diabetes may be more prone to skin infections, dry skin, and slow wound healing. Protect your skin by using sunscreen, wearing protective clothing, and staying in shaded areas when possible.
Staying Hydrated with Type 1 & Type 2 Diabetes
 Adequate hydration is crucial for everyone, but it holds even greater significance for individuals living with diabetes, especially during the hot summer months. Hydration helps maintain optimal blood sugar levels, supports kidney function, and promotes overall well being. When you're well hydrated, it is easier to manage diabetes effectively and prevents complications associated with dehydration.
Adequate hydration is crucial for everyone, but it holds even greater significance for individuals living with diabetes, especially during the hot summer months. Hydration helps maintain optimal blood sugar levels, supports kidney function, and promotes overall well being. When you're well hydrated, it is easier to manage diabetes effectively and prevents complications associated with dehydration.
Tips for Ensuring Proper Hydration
- Drink plenty of water: Make water your go-to beverage and aim to drink it throughout the day. Set a goal to consume at least eight 8-ounce glasses of water daily. If you're engaging in physical activities or spending time outdoors, increase your water intake accordingly. If you find it challenging to remember to drink water, consider setting reminders on your phone or using apps designed to track your water intake. Consider decorating your water bottle with stickers and charms to reflect your personality, sometimes having a water bottle that you love will help encourage you to drink more.
- Limit sugary drinks and alcohol: Sugary beverages like soda, fruit juices, and sweetened iced tea can cause blood sugar spikes. Similarly, alcohol can impact blood sugar levels and increase the risk of dehydration. Limit your consumption of these drinks, and if you choose to have them occasionally, do so in moderation and account for their effects on your diabetes management.
- Include hydrating foods: Certain fruits and vegetables have high water content and can contribute to your hydration goals. Incorporate foods like cucumbers, watermelon, strawberries, oranges, lettuce, and tomatoes into your diet. These foods not only provide hydration but also offer essential nutrients.
Eat a Balanced Diabetes Friendly Diet
Maintaining a balanced diet is essential for individuals with diabetes as it helps regulate blood sugar levels, manage weight, and promote overall health.
- Fresh Fruits & Veggies: Choose a variety of fresh, seasonal fruits and vegetables as they are rich in fiber, vitamins, and minerals. Some excellent options for summer include berries, melons, cucumbers, leafy greens, and tomatoes.
- Eat Lean Protein: Opt for lean protein sources such as grilled chicken, fish, tofu, or legumes to provide sustained energy and promote satiety.
- Eat Whole Grains: Include whole grains like quinoa, brown rice, or whole wheat bread in your meals to provide essential nutrients and promote better blood sugar control.
- Diabetes Friendly Snacks: Snack on diabetes friendly options such as nuts, seeds, Greek yogurt, or sugar-free popsicles to satisfy cravings while keeping blood sugar levels stable.
- Portion Control: Practice portion control by using smaller plates and measuring serving sizes to avoid overeating. This helps maintain stable blood sugar levels and supports weight management.
- Cut back Processed & Sugary Foods: Limit processed and sugary foods, including sugary beverages and snacks, as they can cause blood sugar spikes and lead to weight gain.
- Eat Healthy Fats: Incorporate healthy fats like avocados, nuts, and olive oil into your diet. They provide essential nutrients and can help improve insulin sensitivity.
Engage in Regular Exercise
 Staying physically active in summer is important for managing diabetes. Regular exercise improves insulin sensitivity, aids in blood sugar control, and enhances cardiovascular health. Suitable activities include walking, swimming, cycling, yoga or Pilates, and dancing. Before starting any exercise routine, consult a healthcare provider. Stay hydrated, check blood sugar levels, wear proper footwear and clothing, and schedule workouts during cooler parts of the day. Learn more about managing diabetes with an active lifestyle.
Staying physically active in summer is important for managing diabetes. Regular exercise improves insulin sensitivity, aids in blood sugar control, and enhances cardiovascular health. Suitable activities include walking, swimming, cycling, yoga or Pilates, and dancing. Before starting any exercise routine, consult a healthcare provider. Stay hydrated, check blood sugar levels, wear proper footwear and clothing, and schedule workouts during cooler parts of the day. Learn more about managing diabetes with an active lifestyle.
Protect Yourself from Sun Exposure
 Excessive sun exposure can disrupt diabetes management, leading to sunburns, skin damage, and increased glucose levels. Protecting the skin from harmful UV rays is crucial for individuals with diabetes to maintain overall health and diabetes control.
Excessive sun exposure can disrupt diabetes management, leading to sunburns, skin damage, and increased glucose levels. Protecting the skin from harmful UV rays is crucial for individuals with diabetes to maintain overall health and diabetes control.
Tips for Sun Protection
- Use Sunscreen: Apply a broad-spectrum sunscreen with a high SPF to all exposed areas of the body. Reapply sunscreen every two hours or more frequently if sweating or swimming.
- Protective Clothing: Wear protective clothing, such as wide-brimmed hats and long-sleeved shirts, to shield the skin from UV rays. Choose lightweight, loose-fitting clothing that covers the skin for an additional layer of sun protection.
- Stay in the Shade: Seek shade during peak sun hours (10 am to 4 pm) to reduce direct sun exposure.
Plan Ahead to Manage Diabetes Successfully this Summer
Summer travel and summer activities can disrupt routine diabetes management in a few different ways. Changes in time zones, meal schedules, and physical activity levels can impact blood sugar control. Access to medical care and availability of diabetes supplies may vary in different locations and may not be reliable. It's important to be prepared and proactive to ensure a smooth travel experience while effectively managing diabetes.
Diabetes Summer Planning Considerations
- Consult with a Healthcare Provider: Before traveling, schedule an appointment with your healthcare provider to discuss your travel plans. They can offer guidance on adjusting medication doses, timing, and any necessary precautions based on your specific needs.
- Carry Enough Medication & Supplies: Pack more than enough diabetes medication, insulin, test strips, and other supplies to account for unexpected delays or loss. Split your supplies between your carry-on and checked luggage to avoid losing everything in case of misplaced baggage.
- Keep Medication & Supplies Easily Accessible: Store your diabetes medication and supplies in your carry-on bag to ensure they are easily accessible during the flight and in case of delays or lost luggage.
- Research Destination & Medical Facilities: Learn about the healthcare facilities at your travel destination. Identify hospitals or clinics where you can seek medical assistance in case of an emergency or unexpected complications.
- Carry Snacks & Glucose Sources: Always have diabetes-friendly snacks and sources of glucose readily available in case of low blood sugar episodes. Pack non-perishable snacks like nuts, seeds, or granola bars to ensure you have options when healthy food choices are limited.
- Inform Travel Companions: Let your travel companions or airline staff know about your condition. They can provide support in case of emergencies or assist you if needed.
- Diabetes Identification Accessories: Wear a medical identification bracelet or necklace that indicates you have diabetes. This helps others recognize your condition in case of emergencies.
Read more about traveling with Type 2 diabetes.
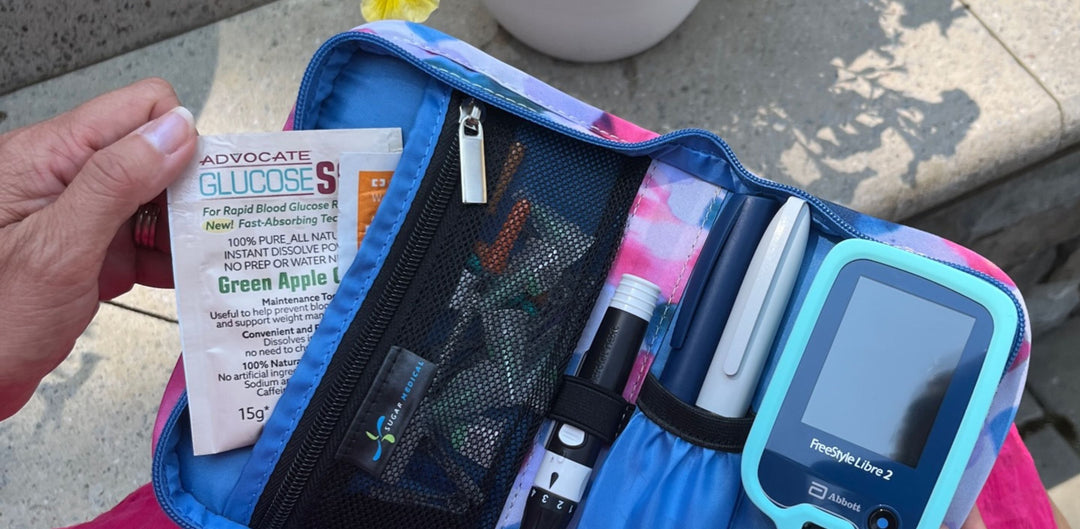
Diabetes Supplies for a Successful Summer
Stay prepared this summer with the right essentials and diabetic supplies. At Sugar Medical, we understand the importance of having reliable and easy to use products to manage your diabetes effectively, especially during the summer months. Our collections include everything you need to stay organized, from blood glucose meters cases and skin adhesives & wipes to nordic ice packs. Our team is dedicated to supporting your diabetes management, allowing you to enjoy the summer season worry free.


Dazzle and shine with this fan favorite this summer! No matter the occasion, this fierce little bag is everything you need to carry your diabetes supplies and daily essentials.
- Insulated back section
- Secure glucose meter with provided hook and loop adhesive patch
- Convenient left and right-handed test strip loop- you choose
- Test Strip Trash Can- holds up to 400+ used strips
- Pocket for 2+ insulin pens, glucose tabs, or pump supplies
- Front pocket for alcohol swabs, medications, and more
- Back pocket for cell phone
- Includes detachable purse strap
- Fits Omnipod®, Medtronic®, and Tandem® pump supplies
- 7" X 4" X 2.75"
INSULATED DIABETES INSULIN SUPPLY CASE


Our Insulated Diabetes Insulin Supply Case is designed to keep your insulin cool and includes one ice pack. The lightweight, stylish case comes with a handle for easy carrying and fits all your diabetic testing supplies in the large back section. Enjoy secure, temperature-controlled storage for your diabetes and other medications.
- Insulated front pocket holds 4 insulin pens or 4 insulin vials
- Exterior slip pocket for ice pack (includes 1 ice pack*)
- Large, zippered pocket for glucose meter, test strips, lancet and more
- 8” X 4.25” X 2.5”
Managing your Type 1 or Type 2 diabetes during the summer requires thoughtful planning and preparation. Staying hydrated, maintaining a balanced diet, staying physically active, practicing sun protection, and planning ahead for travel, can help you navigate the summer season with confidence. With the right mindset, tools, and support, you can enjoy the summer while effectively managing your diabetes, ensuring a season filled with health, happiness, and unforgettable moments. Check out more of Sugar Medical’s diabetes supplies and accessories!








Leave a comment